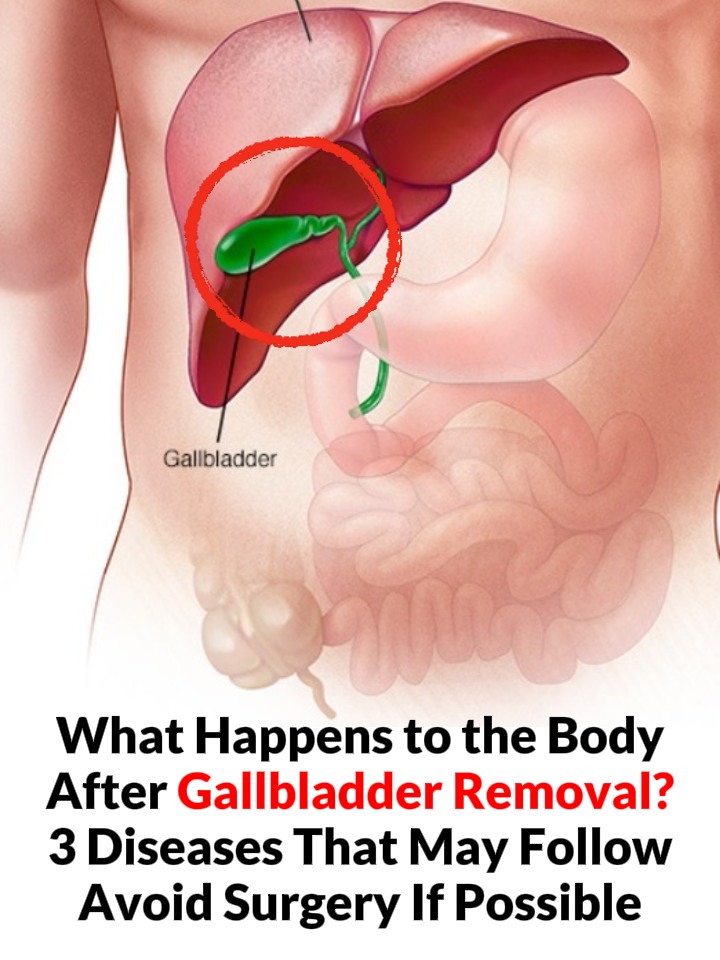
Understanding the Gallbladder: Its Role, Challenges, and Post-Operative Care
The gallbladder is a small, yet crucial organ nestled beneath the liver, intimately linked through the bile duct system. Its primary purpose is to store bile, a digestive fluid produced by the liver. This bile is indispensable for fat digestion. As we indulge in flavorful meals, the gallbladder plays a pivotal role by contracting and releasing bile into the duodenum, where it aids in breaking down dietary fats. This organ does not only function as a storage vessel; it acts as a silent sentinel of our digestive health, ensuring that food is processed efficiently and effectively. Furthermore, bile possesses antibacterial properties, serving as a defense mechanism against harmful bacteria that may disrupt the digestive system. This intricate system exemplifies the harmonious relationship between organs, showcasing how critical the gallbladder is in our overall digestive process.
However, when issues arise with the gallbladder, it can lead to a range of uncomfortable symptoms, including abdominal pain, nausea, and vomiting. Such distress signals indicate that the balance of this intricate digestive system has been disrupted, prompting the need for us to prioritize and protect our gallbladder health. Conditions like gallstones—hardened deposits of digestive fluid—can form in the gallbladder, leading to various complications. But when gallstones are detected, many face a pressing question: should the gallbladder be removed? The answer is not straightforward and heavily relies on the type of gallstones present and the severity of the symptoms experienced. Understanding the options available can empower individuals to make informed decisions regarding their health.
Gallstone Challenges and Surgical Considerations
Gallstones can vary significantly in size, composition, and the symptoms they produce. Some individuals may develop small gallstones without experiencing any symptoms, leading healthcare professionals to recommend a conservative management approach. This approach typically involves regular monitoring rather than immediate surgical intervention. In contrast, for patients experiencing significant discomfort or facing complications such as cholecystitis (inflammation of the gallbladder) or cholangitis (infection of the bile duct), surgical removal of the gallbladder—a procedure known as cholecystectomy—may be necessary. This decision often hinges on individual circumstances, including the type of gallstones, the severity of symptoms, and overall health condition. It’s essential for patients to engage in thorough discussions with their healthcare providers to understand the best course of action.
In some cases, patients may also be educated about non-surgical treatment options, such as medication for dissolving gallstones or endoscopic techniques to remove stones from the bile duct. Nevertheless, these alternatives may not be suitable for everyone, and their effectiveness can vary. Thus, the decision to proceed with surgery is influenced not just by the presence of gallstones but also by the impact they have on a person’s quality of life. The pre-operative assessment often includes imaging tests like ultrasound or CT scans, allowing healthcare providers to visualize the gallstones and evaluate the gallbladder’s condition, leading to more tailored treatment decisions.
The Impact of Gallbladder Removal on Digestion
Following gallbladder removal, patients often experience notable changes in their digestive processes. One of the key alterations is reduced fat digestion ability. Since the gallbladder is responsible for storing bile, its absence may lead to continuous rather than regulated bile flow into the duodenum. This can complicate the digestion and absorption of fats, resulting in discomfort, bloating, and indigestion. For instance, patients might struggle with high-fat meals, experiencing symptoms like diarrhea or cramping, which can be both inconvenient and distressing.
Furthermore, the absence of the gallbladder can disrupt the delicate balance of gut bacteria. Bile contains components that are essential for maintaining a healthy gut flora, and an altered bile flow can lead to an imbalance that might increase the risk of intestinal infections. Some individuals may also experience bile reflux, where bile flows back into the stomach, causing irritation and discomfort due to the acidity and bile salts. This condition can lead to chronic digestive issues if not addressed properly. In such cases, patients might benefit from dietary adjustments and medications to manage these symptoms effectively.
Dietary Adjustments and Health Considerations Post-Surgery
In the wake of gallbladder surgery, dietary adjustments become crucial for maintaining comfort and health. Patients are often advised to start with easily digestible foods, such as liquid or semi-liquid options like lotus root starch or egg custard, which provide necessary energy while reducing the strain on the digestive system. These gentle foods help ease the transition as the body adapts to the changes in fat digestion capabilities. Incorporating high-quality protein sources, including eggs, fish, and dairy, can aid in recovery, supporting bodily functions and healing processes.
Moreover, after the surgery, individuals may find it beneficial to include whole grains in their diet to bolster their immune system. Foods rich in fiber, like peanuts, sunflower seeds, and nuts, are recommended for their nutritional benefits, provided they are consumed in their natural forms rather than fried or processed varieties. These dietary changes can help alleviate potential complications associated with gallbladder removal. Gradually reintroducing more complex foods, while listening to the body’s responses, is critical in the post-operative phase, allowing individuals to regain normalcy while protecting their digestive system.
Long-Term Risks and Recovery Considerations
Despite the essential benefits of gallbladder removal, there are several potential long-term risks that patients should be aware of. For instance, individuals may experience conditions such as reflux gastritis, where the lack of concentrated bile can hinder digestion, especially when consuming rich or fatty foods. This may lead to bloating, diarrhea, and discomfort during meals. Additionally, research indicates an increased risk of colon cancer following gallbladder surgery, as altered bile acid levels can irritate the colon and promote cancerous changes. It underscores the importance of regular medical check-ups and screenings post-surgery, as early intervention can play a crucial role in mitigating these risks.
Another concern is the development of stones in the common bile duct after the gallbladder has been removed. The absence of the gallbladder can increase pressure in this area, leading to potential blockages. Patients who experience recurrent pain or symptoms similar to those caused by gallstones should consult their healthcare provider promptly. Therefore, it is crucial to weigh the risks and benefits of gallbladder removal carefully, ensuring it is only performed when absolutely necessary to avoid compromising the body’s natural defenses. Awareness of these potential complications can empower patients to take proactive measures to safeguard their digestive health.
Conclusion: Emphasizing Post-Operative Care
Post-surgery, patients should adhere to a careful recovery plan that includes avoiding smoking and alcohol, consuming small and frequent meals, and maintaining a light, easily digestible diet. Staying active, while refraining from strenuous activities, can aid in the healing process. By following these guidelines, individuals can promote their recovery and gradually transition back to their regular diets within a few months. It is advisable to maintain open communication with healthcare providers to monitor any unusual symptoms and adjust dietary plans as needed.
In summary, while gallbladder removal can alleviate discomfort associated with gallstones and other complications, it is essential to consider the long-term implications on digestive health and overall well-being. By understanding the gallbladder’s role and taking proactive steps to manage health post-surgery, individuals can navigate their recovery journey more effectively and with greater confidence. Emphasizing comprehensive care, including dietary adjustments, regular medical check-ups, and symptom management, is vital for optimizing health outcomes following gallbladder surgery.