Understanding Nocturnal Symptoms of Diabetes
Many people are unaware that certain symptoms of diabetes can manifest at night, creating a range of **uncomfortable experiences** that might signal an underlying health issue. If you find yourself waking up feeling excessively thirsty, needing to use the bathroom frequently, or sweating profusely without reason, it is crucial to pay attention to these signs. Such nocturnal symptoms can serve as an indication of fluctuating blood glucose levels, a hallmark of diabetes, which can escalate if left unaddressed. Here’s a closer look at the common symptoms, the physiological mechanisms behind them, and proactive steps you can take to manage these nighttime disturbances.
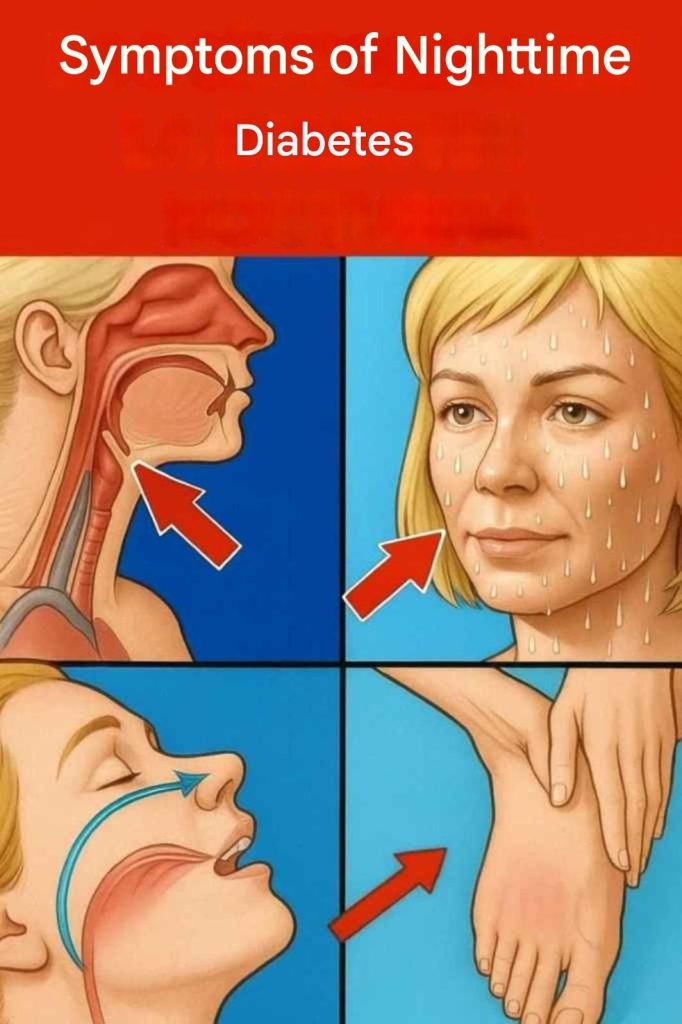
Nighttime Symptoms of Diabetes
The symptoms of diabetes can vary significantly from person to person, but several key indicators often emerge during the night. Understanding these symptoms is essential for early detection and management of the condition. Let’s explore some of the common nocturnal symptoms that individuals with diabetes might experience:
Nocturnal Polyuria: This condition describes the frequent need to urinate during the night, often leading to disrupted sleep. Imagine trying to enjoy a peaceful night only to be interrupted by multiple trips to the bathroom. This symptom can be likened to a faucet that won’t turn off, indicating that the kidneys are working overtime to eliminate excess sugar from the bloodstream. As glucose levels rise, the kidneys filter out the excess, leading to increased urination. In a study published in the journal Diabetes Care, it was noted that patients with uncontrolled blood sugar levels reported nocturnal polyuria as one of the most disturbing aspects of their condition, affecting their overall well-being.
Excessive Thirst: It’s normal to feel thirsty, especially before bed. However, if you find yourself waking up multiple times at night desperately needing to drink water, it could be a sign of hyperglycemia, or high blood sugar levels. This sensation of thirst, known as polydipsia, is the body’s attempt to compensate for dehydration caused by frequent urination. The connection between high blood sugar and increased thirst can be explained by the osmotic effect of glucose in the bloodstream: as glucose levels rise, the body pulls water from tissues to dilute the sugar, leading to an increased demand for hydration.
Nocturnal Sweats: Waking up soaked in sweat for no apparent reason can be alarming. This phenomenon can be linked to hypoglycemia, or low blood sugar levels, occurring during the night. When glucose levels drop too low, the body may activate its fight-or-flight response, releasing adrenaline, which can cause night sweats. This response can disrupt sleep patterns and leave individuals feeling fatigued in the morning. According to endocrinologists, managing these fluctuations is essential, as persistent hypoglycemia can lead to a dangerous cycle of sleep disturbances and daytime fatigue, severely impacting quality of life.
Increased Hunger: If you find yourself waking up in the middle of the night feeling extremely hungry, this could indicate a glucose imbalance. The body requires a steady supply of glucose for energy, and if levels drop unexpectedly during the night, it may trigger intense cravings as it seeks to replenish lost energy. This symptom is particularly prevalent among individuals who may have missed a meal or have not consumed adequate carbohydrates throughout the day, leading to a rebound hunger at night. Research has shown that balanced meals and appropriate carbohydrate intake can mitigate these hunger pangs.
Sleep Disturbances: A lack of stable glucose levels can interfere with your sleep quality. Those with diabetes often experience insomnia or restless nights, as fluctuations in blood sugar can prevent the body from entering deeper, restorative sleep stages. This not only affects your energy levels the next day but can also exacerbate the symptoms of diabetes over time. Studies indicate that poor sleep can lead to insulin resistance, further complicating the management of diabetes. Improving sleep hygiene practices, such as maintaining a cool, dark environment and reducing screen time before bed, can help mitigate these issues.
Why Diabetes Disrupts Sleep
Think of your body as a finely-tuned orchestra, where each instrument must play its part in harmony. In the case of diabetes, certain instruments—representing bodily functions—struggle to stay in tune due to issues with insulin and blood sugar management. The result is a cacophony of symptoms that can interrupt your nightly rest. Blood glucose levels naturally fluctuate throughout the night, but for those with diabetes, these fluctuations can be particularly erratic, leading to episodes of both hyperglycemia and hypoglycemia. This rollercoaster effect can cause multiple awakenings, undermining the quality of sleep that is vital for overall health.
Moreover, the relationship between diabetes and sleep is bidirectional. Not only can diabetes lead to sleep disturbances, but poor sleep can also contribute to worsening blood sugar control. According to research published in the journal Sleep Medicine Reviews, individuals with sleep disorders, such as sleep apnea, are at a higher risk of developing type 2 diabetes. This creates a vicious cycle where managing one condition can significantly impact the other, emphasizing the importance of holistic health approaches.