Understanding Eye Floaters: A Closer Look at This Common Visual Experience
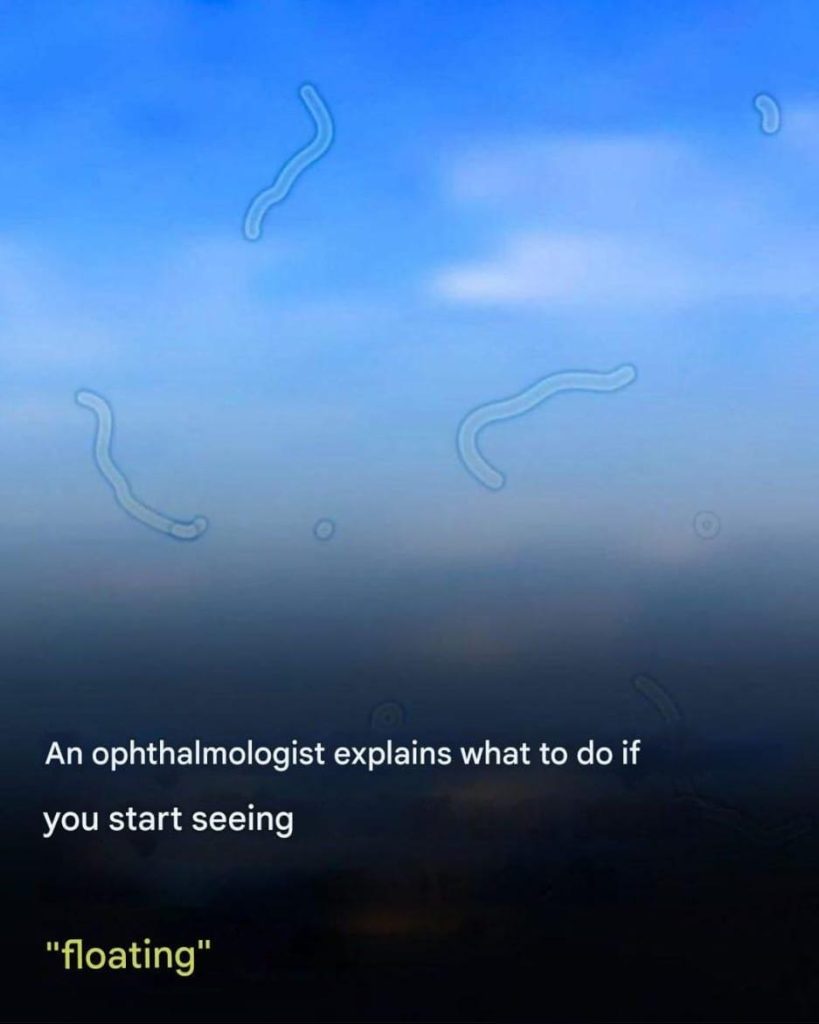
When you gaze at a clear blue sky or a blank wall, you might notice what appear to be small specks, shadowy shapes, or even fine strands floating across your field of vision. These phenomena, often referred to as eye floaters, can be quite distracting. While generally considered harmless, gaining a deeper understanding of floaters is essential for discerning when it may be necessary to seek medical advice. This article aims to unravel the complexities behind eye floaters, exploring their causes, implications, and management strategies.
What Exactly Are Eye Floaters?
Eye floaters are essentially tiny shadows that occur within the eye. They are not visual artifacts residing on the surface of the cornea; rather, they exist within the eye’s interior structure. The eye is primarily filled with a gel-like substance known as vitreous humor. This transparent gel plays a crucial role in maintaining the shape of the eye and allowing light to pass through to the retina. As we advance in age, this gel tends to liquefy, and microscopic collagen fibers can begin to cluster together. These groups of fibers ultimately cast shadows on the retina—the light-sensitive layer located at the back of the eye. Our brain translates these shadows into the drifting shapes we recognize as floaters.
Interestingly, eye floaters can come in various forms. Some floaters may appear as small dots or specks, while others may resemble cobwebs or thread-like strands. The variation largely depends on the size and shape of the clumped collagen fibers within the vitreous humor. Additionally, floaters can be more noticeable against a bright background, such as a blue sky or a white wall, making them more perceptible at certain times than others.
Who Is at Risk of Developing Floaters?
While anyone can encounter eye floaters, certain demographics are more predisposed to experiencing them. The likelihood of floaters increases with age, particularly in individuals over the age of 50, as the vitreous gel undergoes natural changes. Other groups that may be more susceptible include:
- Nearsighted individuals: Those with myopia are more likely to experience floaters due to changes in the shape and structure of the eye. The elongation of the eyeball can cause the vitreous to pull away from the retina more easily.
- People who have undergone cataract surgery: Surgical alterations in the eye can lead to changes in the vitreous humor, making floaters more common.
- Diabetics: Diabetes can impact various aspects of eye health, increasing the risk of floaters. Diabetic retinopathy, a complication of diabetes, can also contribute to the development of floaters.
- Individuals with a history of eye inflammation or trauma: Past injuries or inflammatory conditions can trigger the development of floaters. Conditions such as uveitis or a previous retina injury can make one more prone to experiencing floaters.
When Should You Seek Professional Help?
For the majority of individuals, floaters are a benign aspect of aging and do not warrant concern. However, there are critical symptoms that may signal a significant eye issue requiring immediate medical attention. You should contact an ophthalmologist if you experience any of the following:- A sudden influx of new floaters: Particularly if you notice many floaters appearing simultaneously. This could indicate a change in the vitreous gel that may pose risks to your vision.
- Flashes of light: These may appear as fleeting, lightning-like streaks in your peripheral vision, even in well-lit environments. Flashes can suggest that the vitreous is pulling on the retina, which could lead to tears or detachment.
- A shadow or curtain in your vision: This may manifest as a dark area that encroaches upon your peripheral vision, indicating possible retinal detachment, a serious condition that requires immediate intervention.
- A notable increase in floaters following an eye injury: This could be indicative of a retinal tear or detachment, which is a medical emergency. Any trauma to the eye should be evaluated by a professional to prevent further complications.